As they race to devise a vaccine, researchers are trying to ensure that their candidates don’t spur a counterproductive, even dangerous, immune system reaction known as immune enhancement.
The teams of researchers scrambling to develop a coronavirus disease 2019 (COVID-19) vaccine clearly face some big challenges, both scientific and logistical. One of the most pressing: understanding how the immune system interacts not only with the pathogen but with the vaccine itself—crucial insights when attempting to develop a safe and effective vaccine.

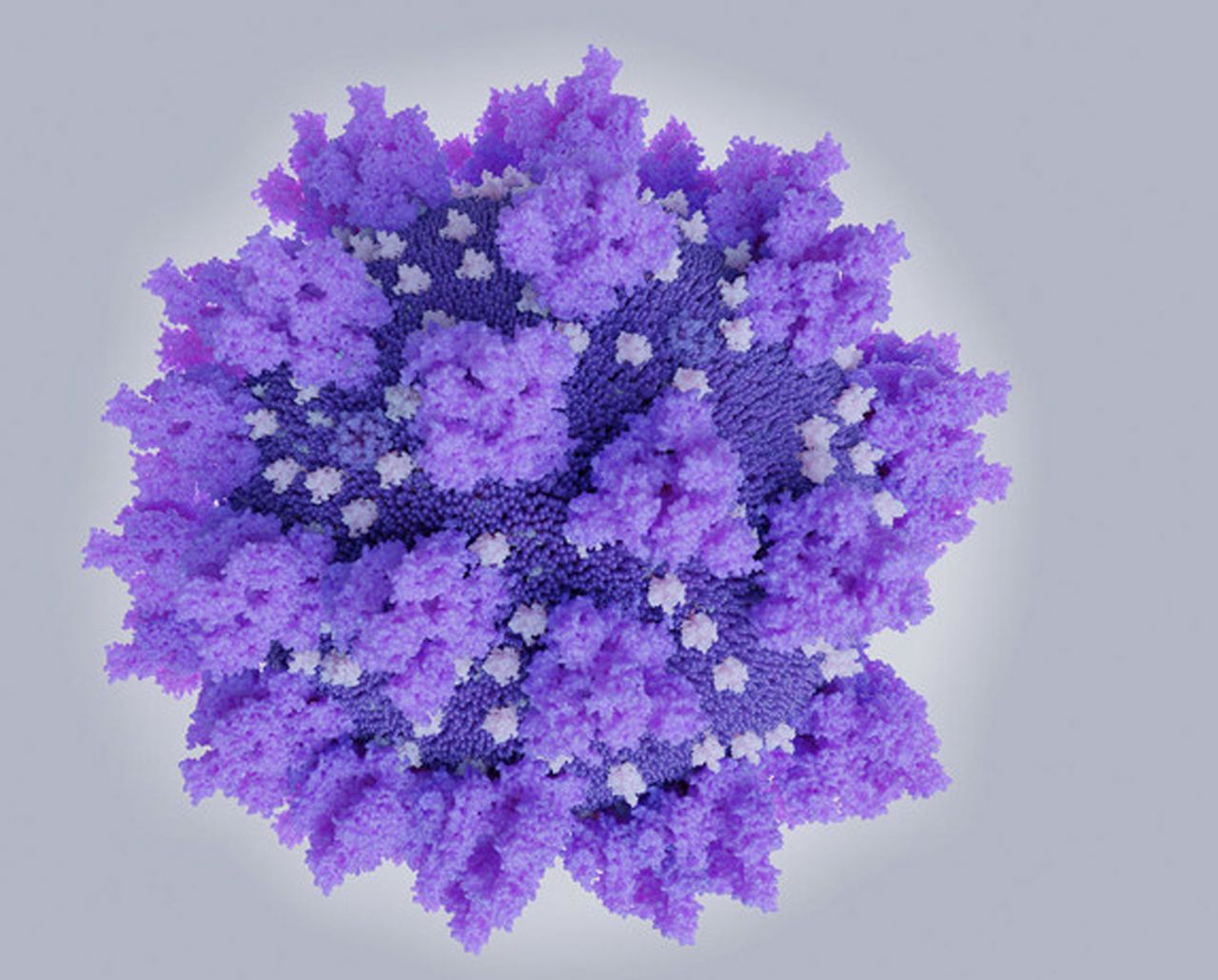
SARS-CoV-2—the virus that causes COVID-19 and the focus of numerous vaccine development efforts—has three surface proteins attached to a lipid bilayer, as seen in this illustration based on X-ray diffraction data. Image credit: Science Source/Juan Gaertner.
Researchers need to understand in particular whether the vaccine causes the same types of immune system malfunctions that have been observed in past vaccine development. Since the 1960s, tests of vaccine candidates for diseases such as dengue, respiratory syncytial virus (RSV), and severe acute respiratory syndrome (SARS) have shown a paradoxical phenomenon: Some animals or people who received the vaccine and were later exposed to the virus developed more severe disease than those who had not been vaccinated (1). The vaccine-primed immune system, in certain cases, seemed to launch a shoddy response to the natural infection. “That is something we want to avoid,” says Kanta Subbarao, director of the World Health Organization Collaborating Centre for Reference and Research on Influenza in Melbourne, Australia.
This immune backfiring, or so-called immune enhancement, may manifest in different ways such as antibody-dependent enhancement (ADE), a process in which a virus leverages antibodies to aid infection; or cell-based enhancement, a category that includes allergic inflammation caused by Th2 immunopathology. In some cases, the enhancement processes might overlap. Scientific debate is underway as to which, if any, of these phenomena—for which exact mechanisms remain unclear—could be at play with the novel coronavirus and just how they might affect the success of vaccine candidates.
A vaccine is designed to boost our natural immune response to an invading virus by priming it to recognize antigens, unique molecules found on the surface of pathogens. Ideally, the immune system responds to the presence of these antigens by producing special immune cells that directly attack the pathogen, or by producing proteins called antibodies. Antibodies attach to an antigen and attract immune cells that engulf and destroy the pathogen. A dysregulated immune response may involve antibodies or immune cells—or both.
Some researchers argue that although ADE has received the most attention to date, it is less likely than the other immune enhancement pathways to cause a dysregulated response to COVID-19, given what is known about the epidemiology of the virus and its behavior in the human body. “There is the potential for ADE, but the bigger problem is probably Th2 immunopathology,” says Ralph Baric, an epidemiologist and expert in coronaviruses—named for the crown-shaped spike they use to enter human cells—at the University of North Carolina at Chapel Hill. In previous studies of SARS, aged mice were found to have particularly high risks of life-threatening Th2 immunopathology (2). Baric expresses his concern about what that might mean for use of a COVID-19 vaccine in elderly people. “Of course, the elderly are our most vulnerable population,” he adds.
Experts generally agree that animal experiments and human clinical trials of candidate vaccines for COVID-19, which is caused by the novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), should include a careful assessment of possible immune complications before releasing the vaccine to the public. If any of the mechanisms under investigation are indeed involved, they say, the resulting risks are real. “You really have to test a vaccine carefully,” says Marc Lipsitch, an epidemiologist at the Harvard Chan School of Public Health in Boston, MA, “and not just roll it out because people are clamoring for it with an epidemic underway.”
Picking the Right Problem
Upwards of 80% of patients who contract COVID-19 develop only mild flu-like symptoms. “The immune system fights off the virus and people might hardly notice,” says Darrell Ricke, a researcher with the MIT Lincoln Laboratory’s Bioengineering Systems and Technologies Group in Lexington, MA, who posted a preprint in March on the possible COVID-19 vaccine risks (3). “But there seems to be a tipping point: Some individuals appear equally healthy yet can progress to a more severe disease.”
Ricke points to ADE as a potential explanation for this variability. The phenomenon has been reported in some tissue culture and animal studies of HIV, influenza, and SARS. But it is best known for its influence on the immune response to the dengue virus. If a person is infected with one of dengue’s four serotypes, their immune system should confer lifelong protection against that serotype. But as researchers have discovered, if that person is later infected by a different dengue serotype, then they can develop a severe and potentially deadly illness. In fact, according to one study in the 1980s, more severe responses were found to be 15 to 80 times more likely in secondary dengue infections than in primary infections (4). Instead of the antibodies neutralizing encountered dengue viral proteins, they enhance uptake of the virus. The back end of the antibody binds to macrophages, a type of white blood cell, and helps the virus enter those cells and accelerate viral replication.
ADE has posed a similar challenge in the creation of vaccines for infections including dengue and a cat coronavirus, feline infectious peritonitis virus (FIPV). In one study, cats vaccinated against FIPV got sicker than cats left unvaccinated (5). Again, the virus-specific antibody increased the virus uptake by macrophages.
Yet some experts doubt that ADE is relevant for COVID-19. “We have no evidence that ADE is actually occurring in human patients,” says Angela Rasmussen, a virologist at Columbia University Mailman School of Public Health in New York, citing such findings.
In principle, anecdotal reports of COVID-19 reinfections in China (6) could lend credence to relevance of ADE—that is, the production of antibodies to the virus (resulting from immunization or an initial natural infection) ends up enhancing entry of the virus into cells. But Rasmussen and other experts underscore the lack of real evidence for COVID-19 reinfections. Any repeat cases so far reported, they say, could be explained by false negative tests between the positive tests. “It’s not clear that patients were ever not infected,” says Rasmussen.
And there is some preliminary experimental evidence casting doubt on ADE. Two papers published in March in Cell show that antibodies against the original SARS infection, which emerged in China in 2002, could also block entry of SARS-CoV-2 into human cells. Another preprint study showed that rhesus macaques infected with SARS-CoV-2 and allowed to recover were not infected after a second exposure to the virus. Unless future data correlate severe COVID-19 cases with original SARS infections—or other diagnostic, pathology, or clinical findings indicate ADE—then there is “not much to go on that suggests ADE is a factor,” Rasmussen says.
Barney Graham, deputy director of the Vaccine Research Center at the National Institute of Allergy and Infectious Diseases, in Bethesda, MD, which is collaborating with the Cambridge, MA-based biotech Moderna on a COVID-19 vaccine candidate, also questioned the role of ADE. Dengue is a flavivirus, a family of viruses that are known to infect macrophages. FIPV also infects macrophages. ADE is unlikely to occur in the current coronavirus, Graham argues, because it does not target or grow in macrophages. Rather, SARS-CoV-2 primarily infects the respiratory epithelial cells, which present different receptors.
Researchers are debating which, if any, of the phenomena related to immune enhancement could be at play in the case of the novel coronavirus—and just how these phenomena might affect the success of vaccine candidates. Image credit: Shutterstock/PhotobyTawat.
Rogue Responses
Graham emphasizes alternative ways in which a vaccine could potentially induce more serious COVID-19 infections: Th2 immunopathology, in which a faulty T cell response triggers allergic inflammation, and poorly functional antibodies that form immune complexes, activating the complement system and potentially damaging the airways.
Both processes were at play as an unfortunate situation unfolded in the 1960s, according to Graham. Researchers at the time were pursuing a vaccine against RSV, the leading cause of severe respiratory illness in infants. In trials of one vaccine candidate, several children who received the vaccine developed a serious illness when infected with the natural virus (7). Two toddlers died. In this case, researchers noticed severe damage and the unexpected presence of lots of neutrophils and eosinophils, both immune cells, in the children’s lung tissue. A similar inflammatory response was seen in animal models of RSV, in which cytokines, a type of immune cell, had invaded and damaged tissue.
“That really killed RSV vaccines for a generation,” says Peter Hotez, a vaccine researcher and dean of the National School of Tropical Medicine at Baylor College of Medicine in Houston, TX. After more than 50 years of further study, a candidate RSV vaccine is finally back in clinical trials.
When SARS, also a coronavirus, appeared in China and spread globally nearly two decades ago, Hotez was among researchers who began investigating a potential vaccine. In early tests of his candidate, he witnessed how immune cells of vaccinated animals attacked lung tissue, in much the same way that the RSV vaccine had resulted in immune cells attacking kids’ lungs. “I thought, ‘Oh crap,’” he recalls, noting his initial fear that a safe vaccine may again not be possible.
But his team revised their approach. Instead of producing the whole spike protein of the virus, they built just a tiny piece of it—the piece that attaches to human cells, called the receptor-binding domain. Subsequent animal tests showed that this strategy did provide the desired protection without the unwanted immune enhancement. With funding from the NIH, Hotez’s team continued on to manufacture the vaccine and were ready for clinical trials.
False Start
But then they hit a roadblock. The money dried up. By that time, SARS was no longer spreading, and interest in a vaccine had waned. In the face of the current pandemic coronavirus, Subbarao suggests, that “risk–benefit calculation might be very different.”

Indeed, when COVID-19 appeared in China, Hotez took special notice, in part because it belonged to the coronavirus family. “I thought we may be sitting on a valuable vaccine. I think it could partially cross-protect against both viruses,” he says. “And the exciting part is I think we have already partially solved the immune enhancement problem.”
Hotez is currently seeking funding for clinical trials of the original vaccine, while also working to produce a new vaccine for COVID-19. Although the basic machineries of the two coronaviruses are nearly identical, the team will need to make adjustments for the slight differences in receptor-binding domains between SARS-CoV-1 and SARS-CoV-2. Ricke notes that the outer surface of the spike protein has been remodeled by mutations that, over time, have made it a better binder and more infective as an airborne pathogen.
Antibodies produced to bind to the original SARS antigens may not bind as consistently to the new SARS antigens. And that lack of potency could raise the risk of immune enhancement, suggests Graham. Otherwise, he says, the receptor-binding domain approach could be effective.
Hotez and others believe that the vaccine lag for COVID-19 might have been avoided if candidate vaccines for SARS or Middle East Respiratory Syndrome (MERS) had received clinical trial funding years ago. “If we had already had a licensed human coronavirus vaccine, we would be a lot less worried about these safety concerns. Because we don’t have one, we’re in new territory,” says Subbarao. “When we work on pandemic influenza vaccines we have years of experience with influenza vaccines [and] we can build from that.”
Not So Fast
Still, several teams are working in parallel with a diverse set of strategies to develop a potent—and hopefully harmless—vaccine.
Graham’s team is attempting to mitigate the possibility of immune enhancement and maximize the speed of vaccine development by injecting mRNA in order to make a highly precise type of protein. “We know at atomic-level detail that this protein is shaped the right way to elicit the right antibodies to have functional activity against this virus,” says Graham. “These things create the kind of T cell response that will prevent allergic inflammation.” Another perk of gene-based delivery: It can be manufactured rapidly.
Moderna’s mRNA vaccine candidate has progressed at unprecedented speed, thanks in large part to China’s January release of the genetic sequence of the virus. A phase 1 clinical trial began on March 16 in Seattle, WA. “We need to get some answers by next winter so we can at least be more prepared for the winter of 2021–2022,” adds Graham.
But immune enhancement concerns linger. Stanley Perlman, a professor of microbiology and immunology at the University of Iowa in Iowa City, agrees that a good T cell response should sidestep enhancement concerns. He is also part of a special committee convened by the World Health Organization (WHO) to address immune enhancement, which they refer to as vaccine enhancement. The committee now aims to define what exactly this enhancement means, what the relevant issues are for a COVID-19 vaccine, and what to do with that information, notes Perlman. A subgroup of the committee is expected to produce a summary report within a few months.
Given how many vaccine candidates are now in the running, Rasmussen says she is confident that at least one of them will work. “But, by the time they have gone through trials to determine safety and efficacy, will there be the same kind of public will to push this out on the market?” she says. “Will we continue to have government and private industry investments?” The WHO and other health leaders emphasize that it will likely be a year and a half before a vaccine is vetted through trials in animals and humans and ready for dissemination.
Vaccine experts have underscored the need to avoid mistakes from the past, such as the halting of SARS vaccine development. More coronaviruses are likely waiting in wild bats, primates, and rodents, ready to make the jump to humans. “Ecological disruption really increases the odds that we might encounter a pathogen that we’ve never seen before but grows in us just fine,” says Rasmussen.
Published under the PNAS license.
References
1. S. M. Tirado, K. J. Yoon, Antibody-dependent enhancement of virus infection and disease. Viral Immunol. 16, 69–86 (2003).
2. M. Bolles et al., A double-inactivated severe acute respiratory syndrome coronavirus vaccine provides incomplete protection in mice and induces increased eosinophilic proinflammatory pulmonary response upon challenge. J. Virol. 85, 12201–12215 (2011).
3. D. Ricke mR. Malone, Medical countermeasures analysis of 2019-nCoV and vaccine risks for antibody-dependent enhancement (ADE). The Lancet. Preprint posted March 3, 2020.
4. S. B. Halstead, Immune enhancement of viral infection. Prog. Allergy 31, 301–364 (1982).
5. H. Vennema et al., Early death after feline infectious peritonitis virus challenge due to recombinant vaccinia virus immunization. J. Virol. 64, 1407–1409 (1990).
6. L. Lan et al., Positive RT-PCR test results in patients recovered from COVID-19. JAMA; Epub ahead of print (2020).
7. P. L. Acosta, M. T. Caballero, F. P. Polack, Brief history and characterization of enhanced respiratory syncytial virus disease. Clin. Vaccine Immunol. 23, 189–195 (2015).
